Travel burden to eye care is cited as a reason for optometric scope of practice expansion.¹ Nevertheless, prior evidence suggests travel may be of lesser concern for most Americans.² Lee et al.² previously demonstrated the majority of Americans reside within 30 minutes of an ophthalmologist and optometrist using 2010 Census data.² Although a landmark study, their analysis only included primary provider locations and did not allow for interstate travel, thus likely underestimating proximity. Moreover, the source data have become outdated. We apply service area analysis to present an updated nationwide assessment of geographic access to eye care. We also expand on prior studies by characterizing the demographic composition of populations with reduced access.²
A list of U.S. ophthalmologists and optometrists was compiled using the Doctors and Clinicians National File (Centers for Medicare & Medicaid Services [CMS]), updated January 18, 2024.³ Addresses (including satellite) were geocoded onto 2022 Census tract maps (U.S. Census Bureau) using ArcGIS Pro 3.2.2 (Esri).⁴ Tracts were adjoined with tract-level, self-reported demographic data derived from the 2018-2022 5-year estimates of the American Community Survey-an annual survey administered by the U.S. Census assessing a representative sample of American households.⁴
Tract-level demographic variables included proportion of pediatric-aged (i.e., <18 years), Medicare-aged (i.e., ≥65 years), White, Black or African American, Asian, American Indian and Alaska Native, Native Hawaiian and Other Pacific Islander, other race, two or more races, Hispanic or Latino, very low-income (i.e., individuals living below the poverty line), college-educated (i.e., Associate’s degree or greater), privately insured (i.e., ≥1 types of private coverage), publicly insured (i.e., ≥1 types of public coverage), and uninsured residents.⁴
Drive-time service areas with breaks at 15, 30, and 60 minutes were generated for each address with the ArcGIS Service Area Analysis Tool, using traffic conditions from Wednesday, February 21, 2024, at 12:00 PM. Tracts (and the totality of their component populations) were classified according to whether the tract geometric centroid was contained within 15 minutes, between 15 and 30 minutes, between 30 and 60 minutes, or more than 60 minutes of service areas. A threshold of 60 minutes (extrapolated from the Health Professional Shortage Area criteria for primary care) was used to classify census tracts as having adequate (i.e., within 60 minutes) or reduced access (i.e., >60 minutes).⁵
To identify demographic variables associated with reduced access, multivariate logistic regressions were generated (with adequate access as the reference or base outcome) using Stata 18.⁵ (StataCorp); model details are outlined in Table S1 (available at www.aaojournal.org). County proximity classifications were performed by calculating the proportion of a given county’s population residing in tracts previously classified as within 15, 30, or 60 minutes. The county as a whole was then classified as within a given level of proximity (i.e., within 15 minutes, within 30 minutes, within 60 minutes, or >60 minutes) if the population majority (i.e., >50%) was found to reside at the corresponding level of proximity. This study adhered to the Declaration of Helsinki and did not necessitate Institutional Review Board review given use of public data. The requirement for informed consent was waived because of the retrospective nature of the study.
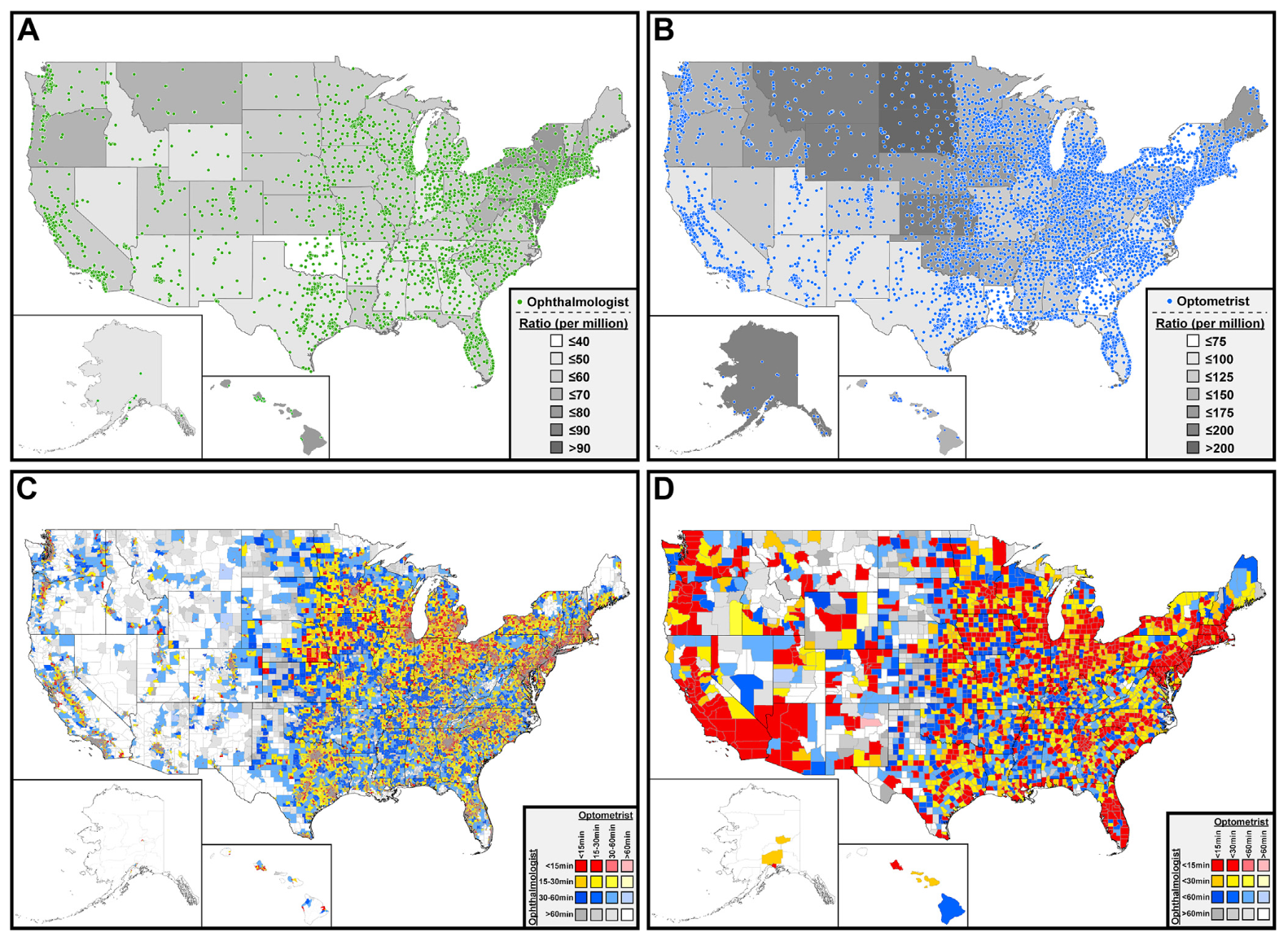
Locations for 17 417 ophthalmologists (30 770 addresses) and 33 291 optometrists (46 099 addresses) were geocoded (Fig 1A and B). There are 52.60 ophthalmologists and 100.55 optometrists per million Americans, with state-level variations depicted in Figure 1A and B. An estimated 74.94%, 90.78%, and 97.80% of Americans reside within 15, 30, and 60 minutes of an ophthalmologist, respectively (Fig 1C); for optometry, the corresponding proportions are 84.52%, 95.16%, and 98.54% (Fig 1C). Aggregate demographic data for tracts according to differential proximity to care are provided in Table S1. Based on multivariate logistic regression, tracts with greater racial and ethnic homogeneity (as measured by a Herfindahl-Hirschman Index [HHI]-like variable, detailed in Table S1) and higher proportions of Medicare-aged and uninsured residents demonstrate significantly higher odds of reduced geographic access (i.e., >60 minutes travel time) to both ophthalmic and optometric care. Moreover, tracts with a greater proportion of college-educated residents exhibit significantly lower odds of reduced access to both types of eye care providers. Although tracts with a greater proportion of pediatric-aged residents exhibit significantly higher odds of reduced access to ophthalmic care, these tracts exhibit significantly lower odds of reduced access to optometric care. Furthermore, tract-level proportion of very low-income residents is not significantly associated with geographic access to ophthalmic or optometric care (statistical data further outlined in Table S1).
There are 212 counties (6.74%) with a population majority (i.e., >50%) within 1 hour of an optometrist but not an ophthalmologist, whereas 8 counties (0.25%) are within 1 hour of an ophthalmologist but not an optometrist. In 166 counties (5.28%) the population majority resides beyond 60 minutes of either provider type (Fig 1D; Tables S2 and S3, available at www.aaojournal.org).
In summary, we demonstrate approximately 98% and 99% of Americans reside within an accessible distance (i.e., 60 minutes) from an ophthalmologist and optometrist, respectively. Our findings update and expand upon those of Lee et al.² who previously demonstrated more than 90% of Americans live within 30 minutes of an ophthalmologist and optometrist. We demonstrate the utility of granular, tract-level geographic data to identify higher-order geographic areas (e.g., counties) that remain beyond a navigable distance from care. These data can, in turn, be used to direct geographically targeted initiatives such as hospital system-backed mobile health efforts or county-sponsored incentives for practice establishment in underserved areas.
We additionally characterize the demographic composition of populations according to differential proximity to care and report characteristics associated with reduced access. Further studies are needed to better understand the drivers and significance of these apparent disparities; these and other inequities should be carefully considered upon deployment of future access-enhancing initiatives, such as teleophthalmology infrastructure expansion and trainee recruitment to ensure more equitable distribution of the benefits of these efforts.⁶
Our study is not without limitations. Proximity is one of myriad factors that can affect access. Only CMS-enrolled providers are included; for each provider, treatment of all ages is presumed, and subspecialization not considered. We cannot account for unequal time spent across primary and satellite locations. Alternative modes of transportation are not considered, and we are unable to account for daily variation in traffic conditions. Although assessment of racial and ethnic diversity using our HHI-like variable helps address collinearity in our regression models, its use precludes evaluation of the unique effects of individual racial and ethnic tract-level proportions on geographic access to care.
Of note, these results are not evidence in favor of optometric scope of practice expansion. First, we demonstrate nearly all Americans reside within a commutable distance from care. Moreover, when compared with optometrists, ophthalmologists have more expertise and training in the medical and surgical management of various eye diseases, which, in turn, may yield improved outcomes.⁷ Thus, the care delivered by each provider is noninterchangeable; efforts should be made to expand the coverage of both types of eye care providers into communities that remain without facile geographic access. Improved characterization of these communities may help inform future health policy, provider recruitment, and care delivery efforts.
AcknowledgmentsThe authors thank the Center for Geographic Analysis at Harvard University and the Clark Library at the University of Michigan for providing the computational resources necessary to perform this study.
JOVANY J. FRANCO, MD¹ROBERTO PINEDA, II, MD²˒³¹ Department of Ophthalmology and Visual Sciences, University of Michigan Kellogg Eye Center, Ann Arbor, Michigan² Department of Ophthalmology, Harvard Medical School, Boston, Massachusetts³ Cornea and Refractive Surgery Service, Massachusetts Eye and Ear, Boston, Massachusetts
Disclosure(s):All authors have completed and submitted the ICMJE disclosures form. The author(s) have no proprietary or commercial interest in any materials discussed in this article.
HUMAN SUBJECTS:Human subjects data were used in this study. This study relies entirely on publicly available data, and thus constitutes non-regulated work per explicit University of Michigan Institutional Review Board policy. All research adhered to the tenets of the Declaration of Helsinki. The requirement for informed consent was waived because of the retrospective nature of the study.No animal subjects were used in this study.
Author Contributions:Conception and design: Franco, PinedaData collection: FrancoAnalysis and interpretation: Franco, PinedaObtained funding: N/AOverall responsibility: Franco, Pineda
Correspondence:Jovany J. Franco, MD, Department of Ophthalmology and Visual Sciences, University of Michigan Kellogg Eye Center, 1000 Wall St., Ann Arbor, MI 48105.E-mail: jovanyf@med.umich.edu
References
- Stein JD, Kapoor KG, Tootoo JL, et al. Access to ophthalmologists in states where optometrists have expanded scope of practice. JAMA Ophthalmol. 2018;136(1):39-45.
- Lee CS, Morris A, Van Gelder RN, Lee AY. Evaluating access to eye care in the contiguous United States by calculated driving time in the United States Medicare population. Ophthalmology. 2016;123(12):2456-2461.
- Centers for Medicare and Medicaid Services. The Doctors and Clinicians National Downloadable File. Published online February 2024. https://data.cms.gov/provider-data/dataset/mj5m-pzi6. Accessed February, 2024.
- Manson S, Schroeder J, Van Riper D, et al. IPUMS National Historical Geographic Information System. Version 18.0. Published online 2023; 2024. https://doi.org/10.18128/D050.V18.0. Available at: https://www.nhgis.org. Accessed February 20, 2024.
- Health Resources and Services Administration of the United States Department of Health and Human Services. Shortage Designation Management System (SDMS): Manual for Policies and Procedures. Published online March 2023. https://programportal.hrsa.gov/docs/pco/Manual-for-Policies-and-Procedures.pdf. Accessed May, 2024.
- Oatts JT, Indaram M, De Alba Campomanes AG. Where have all the pediatric ophthalmologists gone? Pediatric eye care scarcity and the challenge of creating equitable health care access. JAMA Ophthalmol. 2023;141(3):249.
- Stein JD, Zhao PY, Andrews C, Skuta GL. Comparison of outcomes of laser trabeculoplasty performed by optometrists vs ophthalm…
Immune Checkpoint Inhibitor Therapy for Periocular Merkel Cell Carcinoma
Merkel cell carcinoma (MCC) is a rare and aggressive neuroendocrine cancer of the skin with high recurrence, metastatic, and mortality rates compared to other cutaneous malignancies, with a significant rise in incidence from 2000 to 2013.¹ ² Merkel cell carcinoma often demonstrates rapid growth and causes early metastasis, with survival rates significantly worse in patients with metastases.¹ The metastatic rate of eyelid MCC is reported to be 10% to 30%, with a study by our group suggesting a rate of 22%.³
Traditionally, wide surgical excision is the treatment of choice for MCC. Adjuvant radiation is used to improve local control, but periocular radiotherapy is associated with vision-threatening ocular toxicity, particularly when targeting the upper eyelid where MCC is most frequently seen.³ In recent years, the immune checkpoint inhibitors (ICIs) avelumab, pembrolizumab, and retifanlimab have been Food and Drug Administration approved for MCC.
We present 4 patients with locally advanced or metastatic periocular MCC who were successfully treated with ICIs. To our knowledge, these may be the first cases reported of periocular MCC treated with ICIs. This report adhered to the standards set forth by the Declaration of Helsinki. The Institutional Review Board at M.D. Anderson approved this report and waived the requirement for informed consent.
Patient 1 was a 73-year-old woman who presented with a recurrent, large, ulcerating MCC of the right lower eyelid and a large, metastatic mass in the right parotid and neck (Fig 1A, B). She had been heavily treated at an outside facility with chemotherapy and surgery. Magnetic resonance imaging showed anterior orbital infiltration by the mass (Fig 1C). She was treated with pembrolizumab and, given the size and rapid growth of the lesions, concurrent radiotherapy (total dose of 55 Gy) to the right orbit and neck. The patient experienced some improvement after radiation, but significant masses remained (Figure 1D, E). She continued to receive pembrolizumab for a full year and experienced complete resolution of both the periocular mass (Fig 1F) and the metastatic neck mass. She is under continued surveillance at the time of this report and has no signs of local recurrence at 6 months from end of treatment.
Patient 2 was a 52-year-old man who presented with a biopsy-proven right upper eyelid MCC. A preoperative single photon emission computed tomography/computed tomography scan showed drainage to the right preauricular/superficial parotid node (Fig S2, available at www.aaojournal.org). The patient underwent excision of the upper lid mass and had a sentinel lymph node biopsy, which was positive for metastasis. The right upper lid defect was repaired with a Cutler-Beard flap. The patient completed 50 Gy of radiation to the right neck and parotid gland. He was without evidence of disease until 2 years later when he developed a subcutaneous recurrence in his right cheek area, confirmed on biopsy to be in-transit metastatic MCC. He was treated with pembrolizumab and responded with complete…








